Discovering Anaplasma phagocytophilum: a potential threat to pet and human health
In the vast field of pet health care, we are constantly exploring and responding to various factors that may affect the health of pets. Anaplasma phagocytophilum, as a relatively unfamiliar pathogen with great potential threat, is gradually attracting people’s attention. It not only poses a challenge to the life and health of pets, but may also inadvertently pose a threat to human health. Today, let us analyze Anaplasma phagocytophilum in depth and unveil its mysterious veil so as to better protect the health of our pets and ourselves.
Pathogen introduction:
Anaplasma phagocytophilum belongs to the order Rickettsiales, family Anaplasmataceae, genus Anaplasma. It is an obligate intracellular parasitic microorganism that mainly parasitizes in white blood cells, especially neutrophils and monocytes. This special parasitic mode allows it to evade the host’s immune system attack after infecting the host, thereby continuing to reproduce and spread in the host.
From a morphological point of view, the morphology of Anaplasma phagocytophilum is diverse, and it is spherical, rod-shaped or irregular in shape. Its average length is between 0.5 and 1.5 microns, which is relatively small, and its morphological characteristics can only be clearly observed with the help of advanced equipment such as electron microscopes. Its genome is relatively small, but it contains enough genetic information to encode various proteins required for its survival and reproduction. These proteins play an important role in the infection process, such as binding to host cells, invading host cells, surviving and reproducing in cells, etc.
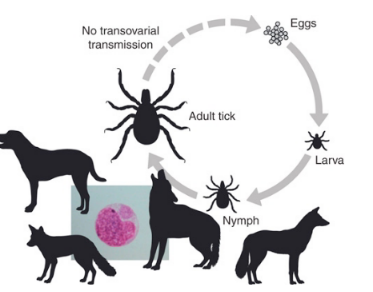
Transmission mechanism
The main vector of A. phagocytophilum is ticks, especially Ixodes ticks. Ticks are common arthropods that are widely distributed in the natural environment. When ticks bite host animals, they inject A. phagocytophilum into the host. Once inside the host, the A. phagocytophilum begins to look for suitable white blood cells to parasitize and multiply in them.
In addition to transmission through tick bites, direct contact with the blood and body fluids of critically ill patients or infected animals may also lead to transmission. For example, if proper protective measures are not taken when handling wounds of infected animals, it is possible to be infected. In addition, laboratory staff also need to be extra careful when handling samples containing Anaplasma phagocytophilum to avoid accidental infection.
Epidemiology
Anaplasma phagocytophilum is distributed worldwide. In my country, it is mainly distributed in mountainous areas, forest areas and grasslands. The natural environment in these areas provides suitable conditions for the survival and reproduction of ticks, thereby increasing the risk of transmission of Anaplasma phagocytophilum. From the perspective of seasonal distribution, the peak of the disease is generally from May to October. During this period, the temperature is high and ticks are active. In a warm and humid environment, the growth and development of ticks are accelerated, and their reproductive capacity is enhanced, which increases the chance of contact with host animals. In addition, during this period, people and pets such as dogs and cats also engage in more outdoor activities, further increasing the risk of infection.
For pets such as dogs and cats, pets of different breeds, ages, and living environments are all likely to be infected. Generally speaking, pets that often go outdoors and come into contact with grass and woods are more likely to be infected with Anaplasma phagocytophilum. For example, working dogs such as hounds and sheepdogs are more likely to be bitten by ticks because they often go out in the wild, so the risk of infection is relatively high. Elderly pets and young pets are also more susceptible to infection because of their relatively weak immune systems. In addition, pets living in areas with dense tick populations, such as those near mountainous areas and forests, will also have an increased chance of infection.
In terms of humans, people who come into contact with ticks and other transmission media are at high risk. Field workers, such as forestry workers, geological prospectors, farmers, etc., are relatively more likely to be bitten by ticks because they often work in natural environments where ticks are present. Camping enthusiasts, hikers, etc. are also likely to come into contact with ticks during outdoor activities. In addition, residents in the epidemic source areas, especially those living in tick-dense areas such as mountainous areas, forest areas, and grasslands, also face a higher risk of infection.
Clinical symptoms
After the pathogen enters the host neutrophils, it may cause delayed apoptosis, prolonged survival time, and enhance the ability of bacteria to survive in the blood. This change in neutrophil function may lead to an increased risk of secondary infection, especially in the case of co-infection with other tick-borne pathogens (such as Ehrlichia). Dogs and cats may show self-limited febrile illness after infection with Anaplasma bacteria. Clinical symptoms include lethargy, fever (up to 41°C), decreased appetite, swollen lymph nodes, and enlarged spleen. For canine pets, symptoms related to polyarthritis such as stiffness, lameness, and muscle pain may occur. This is because infection with Anaplasma phagocytophilum can cause inflammatory reactions in the joints, leading to joint pain and limited movement. In addition, digestive system symptoms such as vomiting and diarrhea are also common.
Some pets may also experience respiratory symptoms such as difficulty breathing and coughing. This may be due to the inflammatory response of the lungs caused by pathogen infection. In severe cases, pets may experience symptoms such as shock and coma, and even be life-threatening.
Test Method
CBC: a commonly used detection method. When infected with Anaplasma phagocytophilum, leukopenia and thrombocytopenia are common manifestations. Leukopenia is mainly caused by the immune response caused by pathogen infection, while thrombocytopenia may be related to abnormal coagulation function caused by pathogen infection. In addition, routine blood test can also observe changes in the morphology and number of red blood cells, which helps to determine whether there is anemia and other conditions.
Urinalysis: In case of infection with Anaplasma phagocytophilum, proteinuria, hematuria, etc. may occur. These abnormal manifestations may be due to kidney damage caused by pathogen infection.
Biochemistry: It can reflect the liver and kidney function, electrolytes and other aspects. In the case of Anaplasma phagocytophilum infection, elevated liver enzymes and kidney enzymes are common manifestations, indicating liver and kidney function damage. In addition, blood biochemical examinations can also observe electrolyte disorders and other conditions, which help to determine the severity of the disease. Blood smears 4-8 days after infection can show intracellular mulberry embryos, which need to be differentiated from Ehrlichia.
Bacterial culture: Isolation of pathogens is the gold standard for confirming infection with Anaplasma phagocytophilum, but the operation is difficult. It is necessary to collect blood, bone marrow and other specimens from patients and culture and isolate them under specific laboratory conditions. Since Anaplasma phagocytophilum is an obligate intracellular parasitic microorganism, the culture and isolation process is relatively complicated and requires professional technical and equipment support.
FIA: Indirect immunofluorescence antibody detection of acute and convalescent serum is a commonly used serological detection method. After infection, specific antibodies will be produced in the patient’s body. By detecting these antibodies, it can be determined whether the infection is caused by Anaplasma phagocytophilum. Acute serum antibody detection is usually performed within 1-2 weeks after onset, and convalescent serum antibody detection is performed 2-4 weeks after onset. If the convalescent serum antibody titer is more than 4 times higher than that of the acute phase, it can be confirmed as Anaplasma phagocytophilum infection.
PCR test: A rapid and sensitive test method. By detecting pathogen nucleic acid in the blood, it can quickly and accurately diagnose Anaplasma phagocytophilum infection. This test method has high sensitivity and specificity, and is particularly suitable for early diagnosis and diagnosis of difficult cases.
Treatment
Antibiotic treatment: Tetracycline antibiotics, such as doxycycline, are preferred. The dosage is usually 10 mg/kg/d for 34 weeks, or 5 to 10 mg/kg, orally, once every 12 to 24 hours for 21 days. In most cases, clinical symptoms disappear 24 to 48 hours after the start of doxycycline. Doxycycline is also an effective treatment drug.
Supportive treatment: During the treatment process, appropriate supportive treatment is also needed, including nutritional support and water supplementation.
Other treatments: If secondary immune-mediated thrombocytopenia occurs, tetracyclines and glucocorticoids should be used for treatment. For pets with more serious conditions, sufficient fluids and electrolytes should be supplemented to maintain water, electrolyte and acid-base balance. Weak or malnourished pets with hypoproteinemia can be given blood transfusions to improve the body’s functional state and enhance the body’s resistance.
In addition, pet owner and medical staff should regularly observe the physical condition of their pets, monitor indicators such as body temperature and heart rate, and promptly detect and deal with abnormal conditions. During the treatment period, the pet should be given enough attention and care to help the pet overcome difficulties.
Preventive measures
Regular deworming: Regular deworming of pets is an important measure to prevent infection with Anaplasma phagocytophilum. You can use special tick anthelmintics and take or apply them to your pet regularly according to the instructions. In addition, you can also wear an insect repellent collar for your pet to enhance the protective effect. Avoid ticks: Try to prevent your pet from entering areas with dense ticks, such as grass and woods. If you must enter these areas, try to shorten your stay and check your pet’s body in time after the activity to see if there are ticks attached.
Regular disinfection: Disinfect your pet’s living environment regularly to reduce the spread of pathogens. Regular physical examinations: Take your pet to the hospital regularly for PCR testing of human-pet co-morbidities, so that you can identify, discover and treat them in a timely manner.
In daily life, we should strengthen our awareness of prevention, avoid tick bites, and promptly detect and treat infection cases. For pet owners, we should regularly deworm their pets, strengthen pet management, improve their immunity, and reduce the incidence of pet infection. For medical workers, we should improve our understanding of Anaplasma phagocytophilum infection, strengthen our diagnosis and treatment capabilities, and provide better medical services for pets.
