Digestive Zoonotic Diseases: Campylobacter jejuni Strikes
In 1906, Campylobacter was isolated from animals and found to be associated with miscarriage and dysentery. Today, it has gradually gained attention from veterinarians. Campylobacter is one of the primary causes of gastrointestinal diseases in pets, potentially leading to symptoms such as vomiting and diarrhea, which significantly impact their quality of life and growth and development. Additionally, as a zoonotic disease, Campylobacter also poses risks to human health.
Pathogen overview
Campylobacter belongs to the genus Campylobacter, family Campylobacteraceae. It comprises a diverse array of species, mainly including Campylobacter jejuni, Campylobacter coli, Campylobacter fetus, Campylobacter lari, Campylobacter upsaliensis, Campylobacter sputorum, Campylobacter helveticus, etc.The main pathogenic species include Campylobacter jejuni, Campylobacter coli, Campylobacter fetus, Campylobacter lari, Campylobacter upsaliensis, Campylobacter salivarius, and Campylobacter hyointestinalis. These species exhibit diverse host ranges and pathogenic potential. Except for Campylobacter jejuni, other subspecies rarely meet both criteria of being zoonotic between pets and humans and causing severe clinical symptoms.Therefore, this article will mainly focus on Campylobacter jejuni.
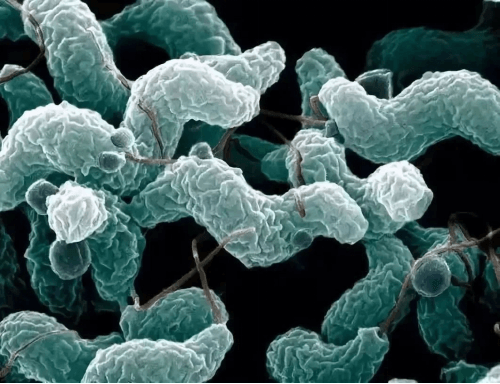
Campylobacter jejuni is a Gram-negative bacterium with a curved, spiral, or S-shaped cell body, measuring approximately 1.5-5 × 0.2-0.5 μm. It has a single terminal flagellum, which is approximately 2-3 times the length of the cell body, giving it active motility. Under a microscope, the bacteria can be observed to move in a jumping or darting manner. It possesses a capsule and does not form spores.
Campylobacter jejuni is a microaerophilic bacterium that thrives in an environment containing 2.5-5% oxygen and 10% CO₂, with an optimal temperature of 37-42°C. It has high nutritional requirements and is difficult to grow on standard intestinal bacterial culture media. It requires a nutrient-rich medium containing blood and serum, and after approximately 36 hours of incubation, it forms small, colorless, translucent, frosted-glass-like colonies. Each colony has a convex center and irregular edges, with no hemolysis observed.
Campylobacter jejuni has weak resistance and is easily killed by drying, direct sunlight, and weak disinfectants. It can be killed at 56°C for 5 minutes. However, in recent years, several drug-resistant strains have been discovered, posing certain challenges to treatment. It is widely distributed in nature and is a normal commensal bacterium in various animals such as cattle, sheep, dogs, and poultry, commonly found in the reproductive tract or intestines of animals. It can contaminate food and water through birth or excrement, thereby threatening the health of pets.

Research indicates that pets, particularly dogs and cats, are important hosts for Campylobacter jejuni. In a six-month study, the prevalence of Campylobacter jejuni was significantly elevated in 304 fecal samples collected from pets, particularly in dogs under one year of age and older dogs. These findings suggest that pets may play a potential role in the epidemiology of Campylobacter jejuni, and close contact between pets and humans may increase the risk of human infection. Additionally, the isolation of pet-specific characteristics may indicate the presence of other pet contamination sources or suggest that pets may serve as reservoirs for Campylobacter. Therefore, veterinarians and pet owners should give sufficient attention to the prevention and control of Campylobacter jejuni.
Epidemiology
The prevalence of Campylobacter jejuni in pets exhibits a high degree of seasonality, particularly during warm and humid seasons. A surveillance study of pet clinic samples found that the average positivity rate for Campylobacter jejuni was 5.36%, while the average positivity rate for Campylobacter coli was 1.79%. In pet breeding facilities and dog samples, the average positivity rate for Campylobacter jejuni was 1.75%. Additionally, the positivity rate for Campylobacter jejuni in young dogs (under 1 year old) was 10.42%, significantly higher than the 1.57% in adult dogs. These data indicate that age is an important factor influencing Campylobacter jejuni infection, with young pets being more susceptible due to their underdeveloped immune systems.
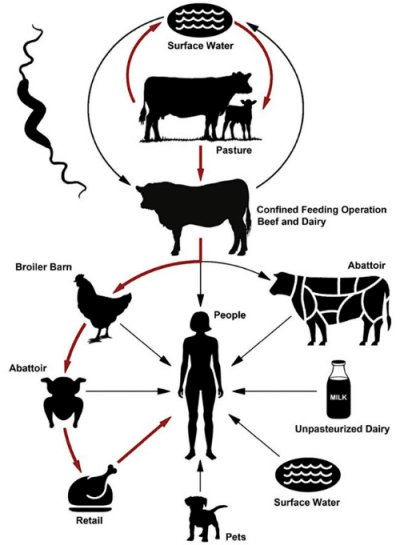
The primary source of infection for Campylobacter jejuni is poultry, particularly chickens, with a carrier rate as high as 50% to over 90%. Additionally, dogs and cats are important sources of infection, especially free-roaming and group-housed dogs and cats, which have the highest fecal isolation rates. The pathogen is excreted through feces, contaminating food, water, feed, and the surrounding environment, and is primarily transmitted through the fecal-oral route. Undercooked meat products and unpasteurized milk are also potential transmission routes. Dogs and cats can become infected with Campylobacter jejuni by consuming these contaminated foods or water. Additionally, direct contact between pets or through contaminated environments is another transmission route. Research shows that close contact between pets and humans may increase the risk of human infection. Therefore, veterinarians and pet owners need to implement effective preventive measures to block transmission routes and protect the health of both pets and people.
Pathological mechanism
Campylobacter infections commonly colonize the jejunum, leading to enteritis symptoms. The pathogenic mechanisms primarily involve flagellum-driven motility, adhesin-mediated adhesion, invasion factors, and toxin production (such as CDT), which is encoded by three tandem genes: cdtA, cdtB, and cdtC. CdtB triggers host cell endocytosis by binding to microfilament proteins (e.g., adhesion proteins) of the cytoskeleton, reorganizing the cytoskeletal structure, and subsequently altering protein function. CdtB is transported to the host cell nucleus via the Golgi apparatus and endoplasmic reticulum, where its DNAse I activity causes double-strand breaks in DNA. CdtB-induced DNA damage disrupts cell division and initiates apoptosis. This activates pro-inflammatory cytokines such as IL-1β, IL-6, and IL-8, as well as the NF-κB signaling pathway via transcription factors. This inflammation causes gastroenteritis, characterized at the cellular level by epithelial cell damage, altering tissue functional capacity and promoting bacterial invasion into underlying tissues, leading to severe diarrhea and loss of nutrient absorption.
Some virulence factors of Campylobacter
Lipid Adhesins
| Virulence Factor | Gene | Function | Feature |
|---|---|---|---|
| CadF (Campylobacter adhesin to fibronectin) | cadF | Binds to host cell fibronectin | Outer membrane protein after binding, promotes Cia protein entry into host cytosol |
| FlpA (Fibronectin-like Protein A) | flpA | Binds to host fibronectin | Outer membrane protein |
| CapA (Campylobacter adhesion protein A) | capA | Involved in colonization and adhesion to epithelial cells | Outer membrane, autotransporter protein with adhesion function |
| HtrA (High temperature requirement A) | hrtA | Cleaves E-cadherin to promote cell invasion | Serine protease; cleaves extracellular domain of E-cadherin to aid invasion and immune escape |
| Peb1,3,4 (Periplasmic binding proteins) | peb 3,4 | Co-acts with CadF to mediate host cell adhesion | Belongs to periplasmic binding protein family |
| JIpA (Jejuni lipoprotein A) | jlpA | Binds to heat shock protein (HSP90α) on epithelial cells | Surface-expressed lipoprotein with multiple binding motifs |
Ⅱ. Invasion-associated Proteins
| Virulence Factor | Gene | Function | Feature |
|---|---|---|---|
| Cia (Campylobacter invasion antigen) | central region | Assists in host cell cytoskeletal rearrangement during invasion | Secreted via T3SS-like system, involved in internalization |
| lomA (Invasion outer membrane protein) | iomA | Invasion | Outer membrane protein |
Ⅲ. Cytolethal distending toxin
| Virulence Factor | Gene | Function | Feature |
|---|---|---|---|
| CDT (Cytolethal distending toxin) | cdtABC | Causes cell cycle arrest and cell death | CdtB is the active subunit; cdtA and cdtC help bind and deliver toxin to host cell nucleus |
Clinical symptoms
Clinical symptoms caused by Campylobacter jejuni infection in pets are quite characteristic. These symptoms not only affect the quality of life of pets, but may also be early warning signs of infection. The following are typical symptoms of Campylobacter jejuni infection in pets:

- Diarrhea: Diarrhea is the most common symptom, and affected pets may experience watery stools or bloody diarrhea. According to a study, cats over six months of age typically have resistance but may become asymptomatic carriers, while puppies and kittens are more likely to exhibit clinical symptoms, such as passing watery stools with a large amount of mucus and bile-like discharge, which may contain blood or white blood cells. Diarrhea may persist for three to seven days.
- Abdominal pain and discomfort: Pets may exhibit abdominal discomfort, such as curling up, frequent licking of the abdomen, or appearing tense and restless.
- Fever: Some pets infected with Campylobacter jejuni may develop fever symptoms, often accompanied by an increased body temperature.
- Vomiting: While not all infected pets will vomit, in some cases, pets may experience vomiting.
- Reduced thirst: Pets may have a reduced desire to drink water, which to some extent reflects their overall discomfort.
- Weight loss: Due to diarrhea and reduced appetite, infected pets may experience weight loss.
- Leukocytosis: An increase in white blood cell count may be observed in blood tests, which is the body’s response to infection.
It is important to note that the clinical symptoms of Campylobacter jejuni infection may resemble those of other intestinal diseases, so accurate diagnosis relies on laboratory testing.
Diagnostic Methods
Laboratory testing for Campylobacter jejuni is a critical step in confirming infection in pets. The following are several commonly used laboratory testing methods:
Fecal sample culture: Traditional diagnostic methods include bacterial culture of pet fecal samples. This process involves inoculating the sample onto selective culture media, such as modified CCD agar and Skirrow blood agar, and then culturing it under microaerophilic conditions. Although this method is accurate, it is time-consuming, typically requiring 24 to 48 hours to obtain results.
Polymerase Chain Reaction (PCR): PCR technology is a rapid and sensitive molecular diagnostic method capable of detecting specific DNA sequences of Campylobacter jejuni in fecal samples. It is particularly suitable for early infection detection and differential diagnosis of multiple pathogens. PCR testing enhances diagnostic efficiency and is currently one of the most widely used laboratory testing methods.
Serological testing: By detecting specific antibodies against Campylobacter jejuni in a pet’s serum, this method can assist in diagnosing whether the pet has been or is currently infected with the pathogen. This method is suitable for pets in the later stages of infection or during recovery, as antibody levels are higher at these stages.
Antigen testing: Using techniques such as immunochromatography to detect Campylobacter jejuni antigens in fecal samples is a rapid screening method. Although its sensitivity and specificity may be lower than PCR, it remains a useful supplementary tool in the absence of molecular biology laboratory facilities.
It is important to note that a single diagnostic method may be inaccurate. The diagnosis of Campylobacter jejuni relies on a combination of medical history, clinical symptoms, and laboratory test results. Veterinarians should use this information, combined with the specific circumstances of the pet, to develop individualized diagnostic and treatment plans.
Treatment Protocol
Campylobacter jejuni infection is typically a self-limiting disease, with most pets recovering on their own within about a week. However, for pets with severe symptoms, antibiotic treatment may be necessary. Commonly used antibiotics include erythromycin, azithromycin, and fluoroquinolones. During treatment, fluid replacement and electrolyte balance are critical to prevent dehydration. Antibiotic type and dosage should be adjusted based on the results of antibiotic susceptibility testing.
Dosage and duration of treatment: The treatment dosage should be adjusted based on the pet’s weight and the drug’s instructions. Generally, the dosage of erythromycin is 10-15 mg/kg, three times daily, for 5-7 days; the dosage of azithromycin is 10 mg/kg, once daily, for 3-5 days. Treatment should continue until the pet’s symptoms have completely resolved for 24-48 hours.
Antibiotic susceptibility testing: Antibiotic susceptibility testing should be conducted prior to initiating antibiotic therapy to determine the sensitivity of Campylobacter jejuni to specific antibiotics. This helps select the most effective antibiotic and reduces the development of antibiotic resistance.
Treatment monitoring: During treatment, the pet’s clinical symptoms and signs should be closely monitored to assess treatment efficacy. If the pet shows no significant improvement in symptoms after 48 hours of treatment, the condition should be re-evaluated, and consideration should be given to changing the antibiotic.
| Drug | Species | Dose(mg/KG) | Route | Interval |
|---|---|---|---|---|
| Erythromycin | Cats, Dogs | 10-15 | PO | 8 |
| Azithromycin | Cats, Dogs | 5-10 | PO | 24 |
| Enrofloxacin | Cats, Dogs | 5 | PO/SC/IV | 24 |
| Chloramphenicol | Dogs | 25-50 | PO/SC/IM/IV | 8 |
| Cats | 10-25 | PO | 12 | |
| Tetracycline | Cats, Dogs | 10-20 | PO | 8 |
| Tylosin | Cats, Dogs | 10 | PO | 12 |
| Cefoxitin | Cats, Dogs | 15-20 | SC/IM/IV | 8 |
In addition to antibiotic treatment, supportive care is equally important for improving your pet’s condition and promoting recovery:
Fluid therapy: For pets showing signs of dehydration, it is crucial to replenish fluids and electrolytes promptly. This can be achieved through oral rehydration salts or, in cases of severe dehydration, intravenous fluid administration.
Nutritional support: Providing easily digestible foods, such as low-fat dog or cat food, can help pets maintain good nutritional status during episodes of diarrhea. In some cases, nutritional supplements or liquid diets may be necessary.
Symptomatic treatment: For pets with fever, physical cooling or nonsteroidal anti-inflammatory drugs (NSAIDs) can be used to reduce fever. For pets with vomiting, antiemetic drugs such as metoclopramide can be used.
Immune modulation: In some cases, immune modulators such as immunoglobulin or interleukin can be considered to enhance the pet’s immunity.
Monitoring and preventing complications: Campylobacter jejuni infection can lead to severe complications, such as Guillain-Barré syndrome. Therefore, neurological symptoms in pets should be closely monitored during treatment, and preventive measures should be taken.
By combining antibiotic therapy with supportive care measures, Campylobacter jejuni infections can be effectively controlled, reducing the occurrence of complications and promoting rapid recovery in pets. For dogs and cats experiencing self-limiting infections, the prognosis for Campylobacter infection is excellent in the absence of systemic complications.
Preventive measures
Daily management and hygiene of pets is the first line of defense against Campylobacter infection. Pet owners should take the following measures to reduce the risk of their pets becoming infected with Campylobacter:
Food safety: Ensure that pet food comes from reliable sources and avoid feeding raw meat and unpasteurized dairy products. All meat products should be thoroughly cooked to kill any pathogens that may be present.
Water hygiene: Provide clean drinking water and avoid letting pets drink from potentially contaminated water sources, such as ponds or untreated well water.
Environmental hygiene: Regularly clean your pet’s living environment, including their bedding, feeding utensils, and toys. Use disinfectants to regularly disinfect areas where pets roam, especially areas that come into contact with pet feces.
Fecal Waste Management: Promptly remove and properly dispose of pet feces to minimize the spread of pathogens in the environment. Wash hands thoroughly after handling feces.
Personal Hygiene: Pet owners should wash hands thoroughly with soap and water after interacting with pets, especially after handling feces, to reduce the risk of pathogen transmission to themselves and family members.
Avoid contact with wild animals: Minimize contact between pets and wild animals, especially those that may carry Campylobacter jejuni, such as wild animals and stray animals.
Regular check-ups: Take pets for regular PCR testing for relevant pathogens to enable early detection and timely treatment.
Campylobacter jejuni, a widely prevalent pathogen, poses a serious threat to the health of pets. Pet owners should remain vigilant, strengthen pet hygiene management, and ensure the healthy growth of their pets. At the same time, veterinarians should continuously improve their professional competence and technical skills to provide pets with higher-quality medical services. Let us work together to create a healthier and safer living environment for pets.
